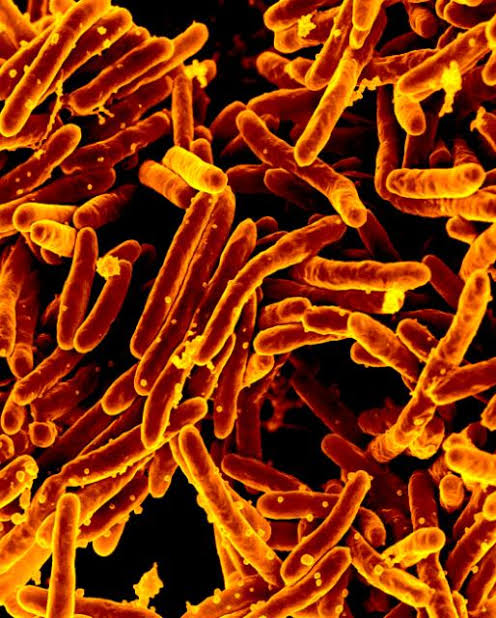
Mycobacterium tuberculosis (Mtb) the pathogen responsible for tuberculosis (TB) in humans causes nearly 1.5 million deaths annually across the globe. Researchers from Council of Scientific and Industrial Research-Institute of Microbial Technology (CSIR-IMTECH), Chandigarh have given a new paradigm to the whole mechanism of how Mtb eludes the treatment. They have discovered that Mycobacterium tuberculosis, which mostly lives within macrophage cells in its human hosts, partly relies on a human drug-efflux protein to evade treatment.
“It is the host factor that might be contributing to drug non-responsiveness which might be passed out as drug resistance. If people just know about the phenotypic and genotypic drug resistance emanating from the bug then they would just assume and ascribe observed drug non-responsiveness to drug resistance, phenotypic or genotypic. Here we have given a new dimension and therefore we say that the cases of drug resistance may be just blown out of proportion” said Dr. Pawan Gupta, lead researcher, CSIR-IMTECH.
The research work is regarding TB bug survival and clearance and in that respect, the team has been able to identify several host nuclear receptors which actually help in the clearance or survival of the bug. Theyfound that nuclear receptors can also play a role in drug non-responsiveness.
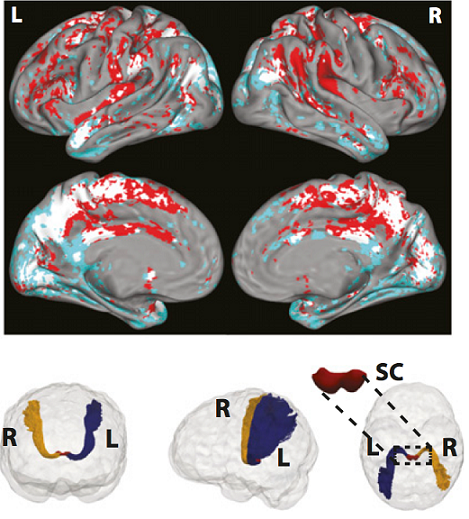
In drug non-responder patients harboring the drug sensitive strain, it has been observed that the expression of the host xenobiotic sensing receptor, Pregnane X receptor (PXR), is high. Xenobiotic receptors mean that it binds to different chemicals which are largely exogenous (drugs, diet, environmental) or could be endogenous present at unusually higher concentration. The xenobiotics have to be constantly cleared out from the body. Liver has an important role in clearing out of these macro molecules. Therefore these receptors generally regulate lot of efflux pump machinery and efflux pump pathway gets activated so they are able to pump out all these toxic chemicals.
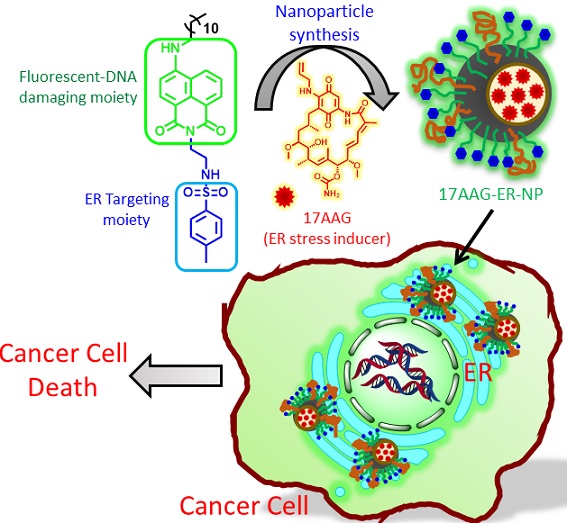
Rifampicin, a well-known antibiotic given for treatment of TB can engage and activate PXR by binding to it. On one hand rifampicin is killing the bug and on the other hand, it is engaging PXR and actually helping in the survival of the bug by two means.
The study shows that there are host factors which are in part responsible for drug non-responsiveness in treatments, such as host nuclear receptor PXR which mediates increase in the efflux pump pathways of host macrophages.
Rifampicin, a well-known antibiotic given for treatment of TB can engage and activate PXR by binding to it. On one hand rifampicin is killing the bug and on the other hand, it is engaging PXR and actually helping in the survival of the bug by two means. First, PXR happens to be a pro-Mtb nuclear receptor as it helps in creating a safe niche within macrophages by promoting foam cell formation, and by reducing cell death and inflammation. Secondly, PXR also leads to up regulation of host efflux pump pathways which effluxes the drug rifampicin too.
“If the drug has to be effective it has to be inside the macrophage then only it would be effective but if it is effluxed out then it would not be effective. PXR induced efflux pump pathways bring about drug non-responsiveness as the drug is no longer effective for killing of the bug because whatever drug was there inside the macrophage get effluxed out” explains Dr. Gupta.
The research work has been published in Journal of Biological Chemistry.
India Science Wire