
Team of researchers
Limbal deficiency is a general terminology used for eye diseases characterised by the deterioration of limbus, limbal stem cells, and their capacity to refill the corneal epithelium by proliferation and differentiation. The consequences experienced by the patients include chronic pain and progressive blindness.
A team of researchers led by Prof. Ashwini Agrawal and Prof. Manjeet Jassal, SMITA (Smart and Innovative Textile Materials) Research Lab, Department of Textile & Fibre Engineering, IIT Delhi, in collaboration with the team from AIIMS Delhi, led by Prof. Radhika Tandon, Department of Ophthalmology, have developed a biopolymer-based scaffold, PCL, as a substitute to HAM (Human Amniotic Membrane) for patients with limbal deficiency.
Human Amniotic Membrane (HAM) transplant is widely used to stimulate epithelial healing in damaged situations. Due to certain limitations in HAM, a cheaper non-biologic substrate was needed to help overcome the constraints. For this, many synthetic substrates have been explored. Polycaprolactone (PCL) has stood out as the best among them. It has a biodegradable aliphatic ester, established drug-delivery models, and is approved by the U.S. Food and Drug Administration. It is used as a bio-engineering scaffold or bone graft substitute.
Polycaprolactone (PCL) scaffolds prepared in IIT Delhi, and modified with plasma treatment, are found efficient. The surface engineering of PCL surface via plasma treatment increased the transparency and biocompatibility. The transparency of the plasma-treated PCL is tested through a water droplet test. The scaffold conversion from hydrophobic to hydrophilic post- plasma treatment providing better cell adhesion is another interesting attribute.
Limbal deficiency is a general terminology used for eye diseases characterised by the deterioration of limbus, limbal stem cells, and their capacity to refill the corneal epithelium by proliferation and differentiation. The consequences experienced by the patients include chronic pain and progressive blindness.
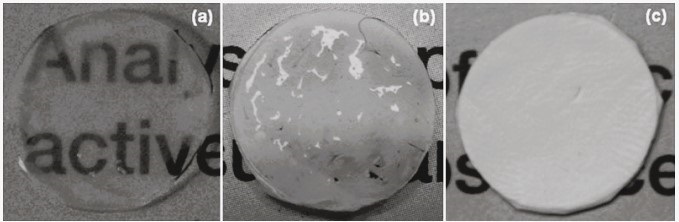
Optical transparency of PCL nanofiber membrane and HAM
Initially, the scaffolds are prepared through an indigenously designed electrospinning setup. The product, electrospun nanofiber, is in the form of thin sheets called a “mat”, ready for plasma treatment. The nano-engineered PCL holds promise to be used as an artificial substrate for ocular surface healing compared to HAM as they require cryopreservation (freezing at a very low temperature), which is not available everywhere.
According to the researchers, the safety and efficacy tests of the plasma-treated PCL (pPCL) scaffolds have shown effective and better healing than HAM, considered the gold standard in scaffolds for tissue engineering.
Limbal epithelial cells (LEC) grown on PCL films showed similar characteristics to those cultured on the glass coverslips and HAM. Tests have confirmed that the plasma-treated poly-ε-caprolactone membrane is safe, biocompatible, and effective in the healing of corneal epithelial defects in rabbits. Pilot clinical trials on humans are underway at AIIMS, New Delhi.
Surface modification of electrospun PCL scaffolds by plasma discharge is an efficient method to make them optically transparent under wet conditions. These highly porous nanofibrous scaffolds with excellent architecture, biocompatibility, and transparency can mimic the natural extracellular matrix. They also assist in maintaining a normal LEC composition.
Consistent efforts and research in the field of tissue engineering will gradually pave a pathway for solving some of the critical health issues in our country and worldwide. It could also help in organ transplantation, one of the significant health challenges due to the increasing wait times.
India Science Wire
ISW/VS/ IIT Delhi/ENG/31/01/2023





